western sky community care timely filing limit
Ambetter is committed to assisting its provider community by supporting their efforts to deliver well-coordinated and appropriate health care to our members. If your prescription cant be filled your pharmacy will give you a notice explaining how to ask us for a coverage decision.
Sign up for Electronic Funds Transfer EFT using the Word or PDF document.
. Check out videos and share a few of them too. Review the application to find out the date of first submission. The same great benefits and coverage you expect with a fresh new feel.
You must fill the prescription at a network pharmacy. If you have any further questions or experience any issues you may reach out to Change Healthcare Support at 800-527-8133 option 1 or send us an email. These policies are subject to change at any time.
BCBS Florida timely filing. If you file a paper return you can get Form 8962 here. The fax number is 1-844-235-6050.
120 Days from DOS. Western Sky Community Care Medical Transportation Western Sky Community Care provides Centennial Care Health Plan members with round-trip rides for appointments to providers for medically necessary services - call 1-844-543-8996 ext. Balance Billing of Community Care Members.
Please note a long-term care pharmacy may provide your prescription drug in small amounts at a time to prevent waste. Timely filing limit is the time duration from service rendered to patients and submitting claims to the insurance companiesfor example if any patient getting services on the 1st of any month then there is a time limit to submit. Our health plans are getting a new look name.
90 Days from DOS. Using these two forms to file your taxes correctly and on time is very important. Care requires that an initial claim be submitted to the appropriate Claims Department under a specific timeline.
If your prescription is written for fewer days we will allow refills to provide up to 30 days at a retail pharmacy and 31 days at a long-term care pharmacy. Protect yourself against Medicare fraud and Identify theft. Validation of data elements on the claim format.
2 member services then ext. Ambetter is also committed to disseminating comprehensive and timely information to its providers through this provider manual regarding Ambetters operations policies and procedures. 180 Days from Initial Claims or if secondary 60 Days from Primary EOB.
Western Sky Community Care is committed to providing solutions for Medicaid beneficiaries throughout New Mexico. 12 Months from DOS. Please check your contract to find out if there are specific arrangements.
Providers must comply with Plan processes to identify access and establish treatment for complex and serious medical conditions. The video library contains a collection of helpful information to help you live your best possible life. If you dont you may lose your tax credit resulting in higher premiums and possible loss of coverage.
For an Insurance company if the initial filing limit is 90 days Claim being submitted after 90th day will be automatically denied by the system for Timely Filing. Potentially unsafe amounts Interactions with other drugs like benzodiazepines A new prescription may be limited to a seven-day supply or less. The phone number is 1-844-543-8996 TTY.
If you have questions please contact Member Services. Western Sky Community Care. 12 Months from DOS.
This limit does not apply if you have been taking an opioid. BCBS timely filing for CommercialFederal. Western Sky Community Care a wholly-owned subsidiary of Centene in partnership with the New Mexico Human Services Department will provide coordinated healthcare long term services and supports pharmacy vision and transportation.
Our new fax number to the Member Grievance and Appeals fax line is. Send it electronically by fax. The filing deadline for your federal taxes is April 18 2022.
The fax number is 1-844-235-6050. Provider ClaimPayment Appeal Rights. CommunityCare Claim Payment Policies - Commercial Products.
This enables providers to easily track their claims. CommunityCares claim payment policies are designed to assist health care providers when submitting claims and provide information on how CommunityCare generally adjudicates a claim for the referenced item or service. Department of Health and Human Services Office of Inspector General is alerting the public about a fraud scheme involving genetic testing.
By the time a claim is successfully received electronically. If you used the erroneous fax number recently WSCC requests you contact Member Services at 1-844-543-8996 for further assistance. Community Care helps you get the behavioral health treatment you need for better health and a higher quality of life.
Allwell will provide you with at least 60 days written notice of termination if electing to terminate our agreement without cause or as described in youParticipation Agreement r if greater than 60 days. 22 rows If claims submitted after the timely frame set by insurances then those claims will be denied by insurance companies as CO 29-The time limit for filing has expired. Whenever claim denied as CO 29-The time limit for filing has expired then follow the below steps.
For any questions or concerns please contact the provider hotline toll free at 1-866-937-2783 option 1 between the hours of 8am to 430pm Monday through Friday Central Time. An EDI claim averages about 24 to 48 hours from the time it is sent to the time it is received.

I Saw A Little Girl About 4 Walk Up To A Man With Biker Hair Who Was Completely Covered In Ta Love Gives Me Hope Faith In Humanity Faith In Humanity Restored
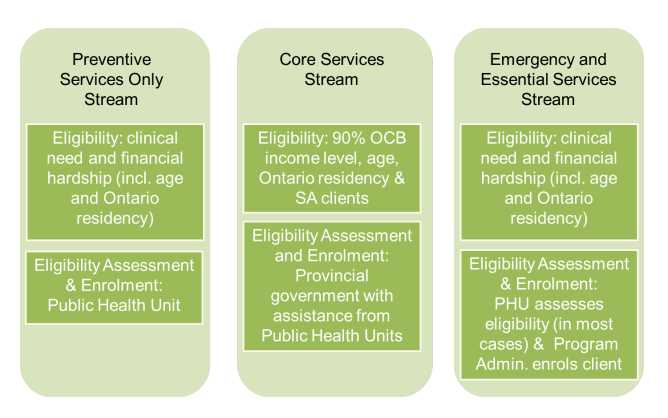
2022 Healthy Smiles Ontario Everything You Need To Know

How To Wax Fall Leaves Ehow Autumn Leaves How To Wash Converse Wax

Pinterest The World S Catalog Of Ideas

-png.png?width=600&name=Community%20Petition%20Download%20(2)-png.png)